As the links between physical health and community wealth and vitality become clearer all the time, fourteen regional and national health systems are coming together to commit at least $700 million to investments in affordable housing and economic development in the cities where they’re located.
The commitment by the Healthcare Anchor Network, a project of the nonprofit research and advocacy organization Democracy Collaborative, will direct the wealth and resources of some of the largest employers in a number of U.S. states to local development projects. The investments will go toward affordable-housing projects, “equitable economic development,” and investments in minority- and women-owned businesses, the group announced. The goal of the effort is for health centers to invest in the health of their communities beyond the care they provide inside hospitals, says Dave Zuckerman, director of the Healthcare Anchor Network.
The health systems include large consortiums of insurance services, hospitals and doctors’ groups like Kaiser Permanente, Einstein Healthcare Network, and Trinity Health. The systems have hospitals and other facilities that are among the largest and wealthiest institutions in cities and towns around the country. The Healthcare Anchor Network launched in 2017 with 11 health systems, and now includes 46, Zuckerman says. Health systems can “leverage their everyday business practices like hiring and supply-chain and investments in a different way, to build more inclusive and sustainable communities,” Zuckerman says.
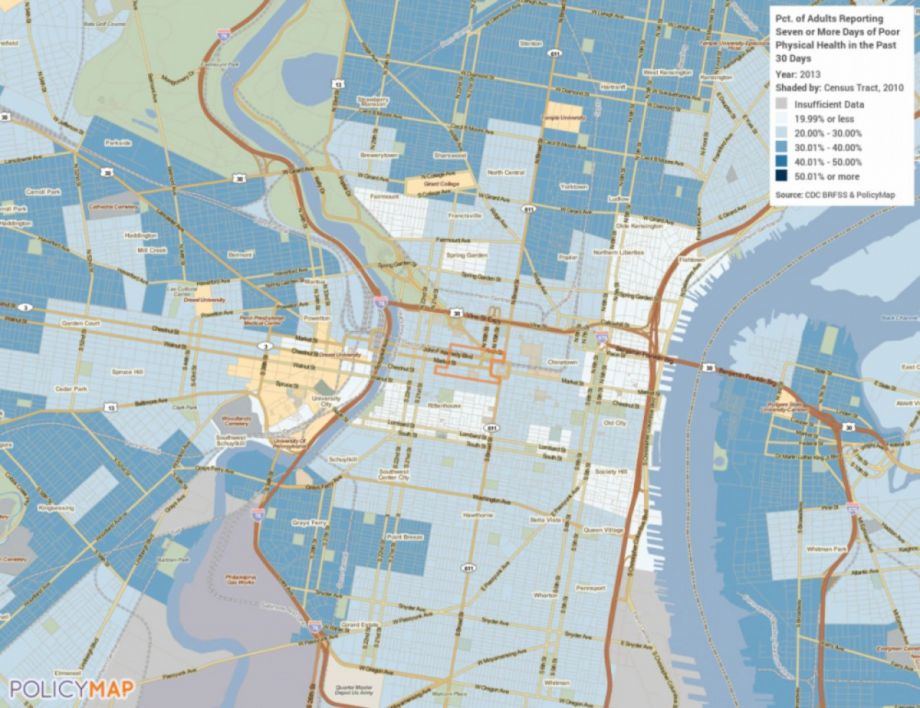
Research shows that health outcomes are “causally related” to income and race, Zuckerman says. As the Urban Institute wrote in one study, “The greater one’s income, the lower one’s likelihood of disease and premature death.” Racial wealth disparities, and racial disparities in healthcare, also contribute to racially unequal health outcomes, research suggests. As the Democracy Collaborative noted in a 2015 report, “Overwhelming evidence from the U.S. Department of Health and Human Services, the Centers for Disease Control and Prevention, and other sources suggests that social, economic, and environmental factors are more significant predictors of health than access to care.” With that in mind, Zuckerberg says, all large institutions should consider how their business practices and financial investments contribute to the health of their communities. For health systems, the link is especially obvious.
The systems are committing to investments that can take a variety of forms, Zuckerman says.
“We aren’t prescribing what the investments should look like, with the exception that they should be in the communities they serve, communities with high health disparities, and they should try to emphasize equity in communities of color, where possible,” Zuckerman says.
In many cases, participating health systems will be making investments through locally rooted Community Development Financial Institutions (CDFIs) that help build affordable-housing and other community-based development projects. Health systems are uniquely positioned to invest in community development projects because improving community health is part of their mission, and because their size gives them access to a lot of resources, Zuckerman says. The investments they’re making are still designed to draw financial returns, but because of their own wealth, health systems can wait for longer-term returns, Zuckerman says.
“How can these systems address market failures and fill market gaps through this patient capital, and not supplant traditional finance but really step in to fill holes in the ecosystem?” he says.
Many health systems have already been making these types of investments, Zuckerman says, and the $700 million accounts for both new commitments and initiatives that some health systems already have in place. It’s always been a goal of the Healthcare Anchor Network and the Democracy Collaborative to push health systems and other institutions toward impact investing, Zuckerman says. It has taken some time to convince some leaders of these systems that investing in local development and housing isn’t an entirely new initiative, but rather tweaking an existing business practice.
“They have to make these investments in stocks and bonds,” Zuckerman says. “The education was to help show them how [the investments] can be leveraged differently.”
The announcement is significant, he says, because it’s the first time a group of large health systems are coming together and announcing publicly and collectively that this type of an investment “is an important thing to do,” Zuckerman says. It’s the type of public commitment that could convince other health systems and institutions to consider making similar investments, with the hope that impact investing becomes standard practice, he says.
Tonya Wells, the vice president of social impact investing and community development at Trinity Health, says that the $700 million announcement includes a $75 million investment that Trinity has already committed. Of that $75 million, the group has already made $36 million in loans and committed $10 million in loans to other projects. Around 43 percent of the loans that have already been made are dedicated to housing projects, either through CDFIs or as one part of a Low-Income Housing Tax Credit deal, Wells says. More than three quarters of the $10 million that Trinity has committed to other projects will be used for affordable housing, she says.
Each of Trinity’s hospital facilities performs a community health needs assessment every three years to determine the types of health challenges its neighborhoods are facing, Wells says. Wells works with Trinity officials locally to determine what kinds of investments to pursue, she says. The group works with more than 20 CDFIs across the country. Trinity was a founding member of the Healthcare Anchor Network.
“We were driven from a mission perspective, but I do believe there is a business model,” Wells says.
Investments can help provide safe, healthy homes for people who might otherwise go homeless or live in substandard conditions, both of which often lead to health problems. Over the long term, Wells says, health systems can expect to see cost savings related to improved health in their communities.
“I think hospitals and health systems are really well poised to engage in this way, of addressing infrastructure in our communities,” Wells says. “We know our patients. We know our communities. We’re credible, and in many cases have strong balance sheets. This is a really important part of how we’re going to address the root causes of poor health.”
The Healthcare Anchor Network will be monitoring the impact of the investments too, Zuckerman says. At first the group will be tracking the dollars dedicated to affordable-housing developments, but eventually, Zuckerman says, it will be able to monitor health outcomes related to the health systems’ investments.
“For now,” he says, “we’re working with the knowledge that we need to work at this intersection of race and wealth in order to be able to move the needle on health disparities.”
This article is part of Backyard, a newsletter exploring scalable solutions to make housing fairer, more affordable and more environmentally sustainable. Subscribe to our weekly Backyard newsletter.

Jared Brey is Next City's housing correspondent, based in Philadelphia. He is a former staff writer at Philadelphia magazine and PlanPhilly, and his work has appeared in Columbia Journalism Review, Landscape Architecture Magazine, U.S. News & World Report, Philadelphia Weekly, and other publications.
Follow Jared .(JavaScript must be enabled to view this email address)